A new HIV vaccine, based on the Moderna COVID-19 inoculation, has shown a 97% antibody response rate in Phase I clinical trials. Currently, HIV affects more than 38 million people globally. If approved, this vaccine could become the first stage of a multi-step strategy to combat HIV and other viral diseases.
The vaccine successfully stimulated the production of rare immune cells needed to generate antibodies against HIV, which causes AIDS and interferes with the body’s ability to fight infections, reported non-profit organisations IAVI and Scripps Research.
“This study demonstrates proof of principle for a new vaccine concept for HIV, a concept that could be applied to other pathogens, as well,” said William Schief, a professor and immunologist at Scripps Research and executive director of vaccine design at IAVI’s Neutralising Antibody Centre (NAC).
The vaccine is meant to act as an immune primer that triggers the activation of cells via a process called “germline-targeting,” according to The European Pharmaceutical Review. Its purpose is to act as the first step in a vaccine regimen that would elicit the production of a variety of broadly neutralising antibodies (bnAbs). Stimulating this type of response has reportedly been pursued in HIV research for decades because it targets a structural aspect of the virus that does not vary much from strain to strain. The surface of HIV cells has proteins called spikes. The vaccine works to disable them from entering human cells.
While a 97% response rate is exceptionally positive, it is important to note that this is representative of an initial study of 48 adult volunteers who enrolled in the trial. Phase I testing marks the first time a vaccine is tested on a small group of adults in order to evaluate its safety and measure immune responses. According to the Centers for Disease Control and Prevention, the next step, Phase II, would be to expand the clinical study and give the vaccine to people similar to those for whom the new vaccine is intended. By Phase III, the vaccine is given to thousands of people to test efficacy and safety before being submitted for a rigorous approval and licensing process. Often, vaccines undergo a Phase IV in which the vaccine would go through a formal, ongoing study even after it’s been approved.
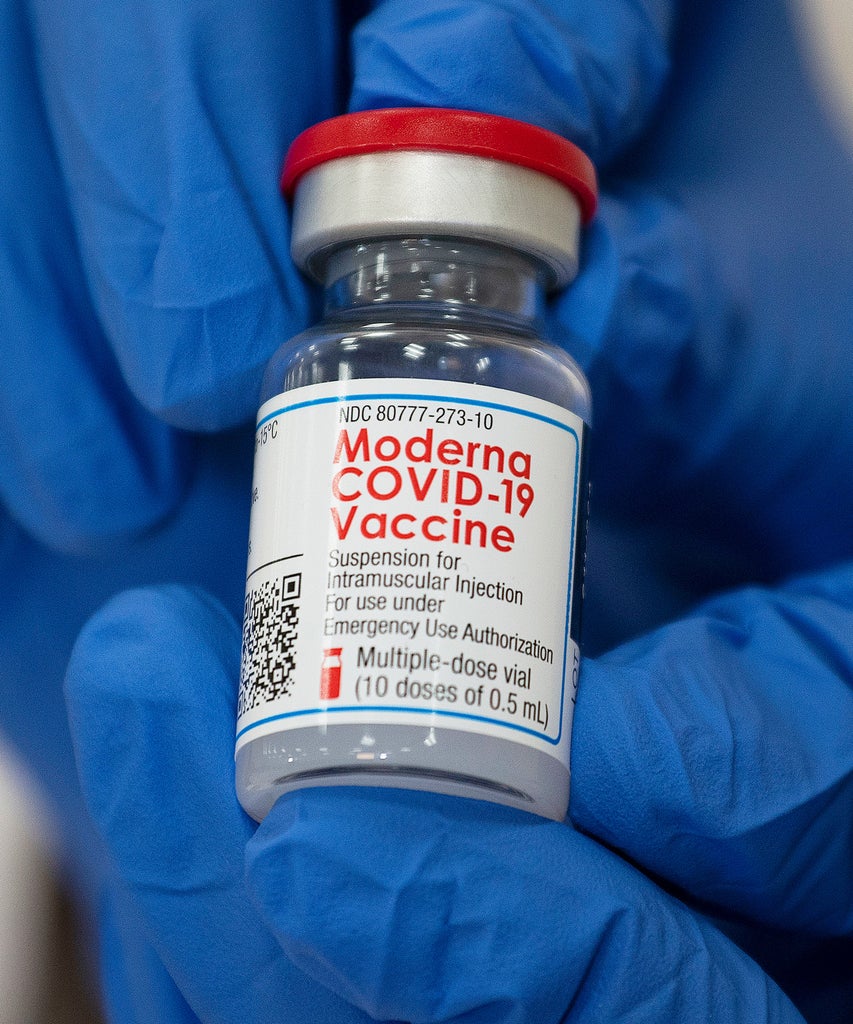
“As a next step, IAVI and Scripps Research are partnering with the biotechnology company Modern to develop and test an mRNA-based vaccine that harnesses the approach to produce the same beneficial immune cells,” the organisations said in a joint statement. “Using mRNA technology could significantly accelerate the pace of HIV vaccine development.”
Like what you see? How about some more R29 goodness, right here?
What Happens If You Get COVID Between Vaccines?