How’s your vaginal microbiome looking today? If it’s never even crossed your mind, you’re not alone. Like much of the inner workings of our bodies, the vaginal microbiome is a fascinating but largely ignored feature. From today though, it’s easier than ever to get a snapshot of what’s going on down there, should you care enough to part with your hard-earned cash.
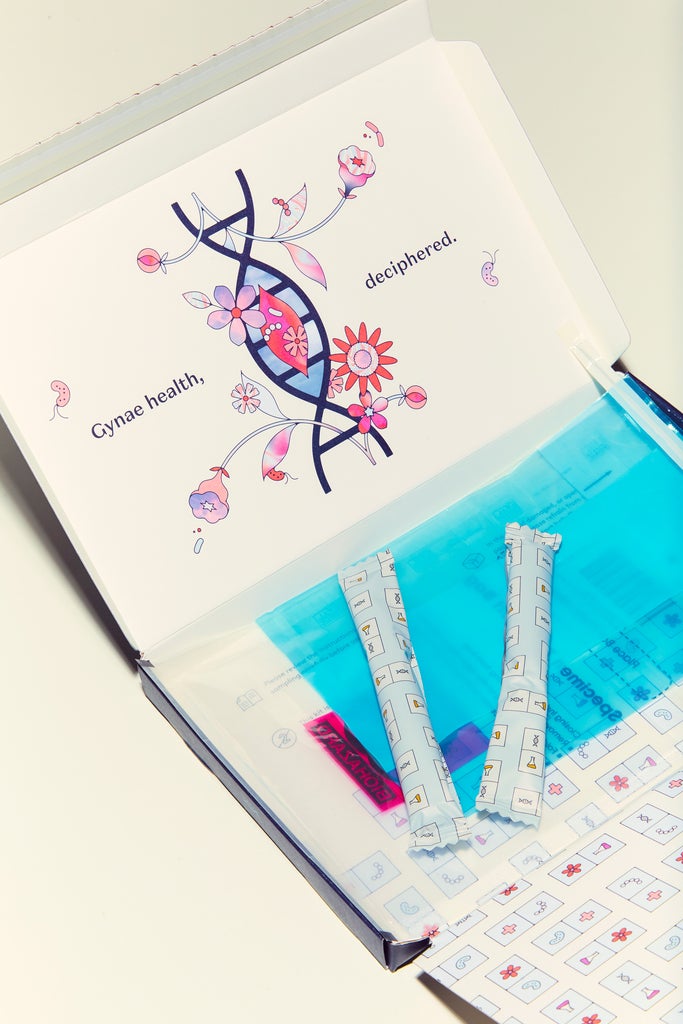
Female-founded gynaecological health startup Daye has launched what claims to be the world’s first tampon-based, at-home vaginal microbiome screening kit. As well as identifying any vaginal infections – like thrush or bacterial vaginosis (BV) – this nine-factor screening test also promises to tell you if your microbiome is disrupted.
I’ve been writing about the gender health gap for years so let me start by saying I’ve got a lot of time for Daye’s ethos, which is all about closing the gender gap in medical research, raising standards in gynaecological health and creating innovative products to help with issues like period pain and vaginal infections. Gynaecological health has always been hugely underserved, both in research and clinical practice, so it’s great to see companies working to change that.
Nevertheless, this one had me scratching my head a little. Is at-home vaginal microbiome screening really something consumers have been crying out for? Should this be something we care about? And how accessible is it really – particularly in a cost of living crisis – at £89.95 for a one-off test or £69.95 for an annual, biannual or quarterly subscription?
Firstly, what do we – by which I mean scientists – actually know about the vaginal microbiome right now? I asked Dr Anita Mitra aka Gynae Geek, a gynaecologist with a PhD in the vaginal microbiome. “Generally speaking, lactobacillus is the bacteria associated with health. Having high levels of lactobacilli is associated with a healthy vagina, while having lower levels seems to increase your risk of STIs, infections, pre-term labour, miscarriage and gynaecological cancers – as Daye rightly says in the marketing for their screening kit,” she explains.
The problem, adds Dr Mitra, is that private companies providing gynaecological health products have become a huge industry. “Companies are skipping a step and saying: ‘If a healthy microbiome is X and an unhealthy microbiome is Y, why don’t we use probiotics to try and manipulate the microbiome?’ This is a very simplistic way of looking at it and I don’t personally believe that Y is always unhealthy. There are lots of different factors that can affect your microbiome. You also can’t say that everybody with an ‘unhealthy’ microbiome is going to get such and such disease and everybody with the ‘normal’ microbiome is not.”
Dr Edward Morris, president of the Royal College of Obstetricians and Gynaecologists, agrees, telling R29: “This test can indicate when a woman’s microbiome may be disrupted – however there are lots of factors that may disrupt the microbiome, and this does not necessarily mean those with a disrupted microbiome will experience fertility problems.”
When it comes to vaginal probiotics (which, incidentally, Daye also sells), Dr Mitra says there is some evidence to suggest that they could one day be used to rebalance disrupted microbiomes but more research is needed. “We don’t really know enough yet about how to manipulate the microbiome. There are certain people who I will recommend probiotics to in hospital, but there isn’t strong evidence to say we should all be taking a probiotic for women’s health,” she explains.
We don’t really know enough yet about how to manipulate the microbiome.
Dr Anita Mitra, Gynae Geek
Specifically, Dr Mitra adds, there’s decent evidence that probiotics can help with recurrent bacterial vaginosis (BV). This is because BV is two things: a depletion of your lactobacillus and an overgrowth of anaerobic bacteria. It’s traditionally treated with antibiotics, which kill the anaerobes, but probiotics can help to try and repopulate the lactobacillus.
There’s less evidence for the use of probiotics to treat thrush, she adds. “In those cases, I would have a sensible conversation with the patient and say that if they want to try it, it’s something they’d have to spend their own money on, and I can’t guarantee it will help. In a few years we might be in a very different place, and I hope we’ll be able to prescribe them to patients, but the science isn’t quite there yet.”
The big question, then, is what can Daye’s screening kit usefully tell us, and will it actually leave consumers with more questions – and anxieties – than answers? Checking for thrush or BV is one thing but there are already £10 high street testing kits that do that. Will screening for other issues simply send women to their GPs, panicking that they’re infertile or going to get cancer?
Crucially, Daye’s founder Valentina Milanova tells me: “We partner with gynaecologists and GPs to provide consultations on the results, and we make it very clear in the results themselves that they are not a medical emergency and people shouldn’t panic over them. The solutions we recommend are often low cost and easy to implement, such as prescription treatments for BV, or lifestyle changes.”
These solutions include providing access to pharmacists to prescribe treatments and practical insights on taking care of your vaginal health, like how to choose the best lubricant or underwear and how your contraception could be linked to vaginal infections or dryness.

“The utility of a vaginal microbiome screen is in understanding your current bacterial composition,” explains Milanova. “This can help you identify the presence of pathogens, which could be causing you recurrent vaginal infections (candida, which causes thrush, or Gardnerella, which causes BV) or preventing you from becoming pregnant (ureaplasma or mycoplasma). If you have suffered recurrent UTIs, you may find a disrupted vaginal microbiome to be the cause. Knowing you have a low lactobacilli count can also help you and your physician make informed decisions on your risk of a recurrent miscarriage or preterm labour.”
Again though, says Dr Mitra, the problem is that there simply isn’t enough evidence to do anything meaningful with this kind of information in a clinical setting.
The testing kit itself does appear to be rooted in decent scientific research which, Milanova says, shows that tampons have a greater diagnostic capacity and that patients find them more user-friendly than other screening methods like swabs or urine samples. “At Daye we believe in building products that are rooted in scientific rigour. This means we never want to get ahead of the science available. Like many other areas of gynaecological health, vaginal microbiome research has been underfunded for decades, which is why it hasn’t gone mainstream yet,” she explains.
In response to Dr Mitra and Dr Morris’ comments, she adds: “By screening your microbiome, you are also contributing to an increased global understanding of the best ways to detect and manage gynaecological health diseases, which in turn helps bridge the gender gap in medical research and innovation. It is incredibly important that we better understand the relationship between the vaginal microbiome and these different gynaecological health conditions. There’s evidence that the microbiome is also associated with vaginal atrophy with menopause, with endometriosis and PCOS, and that’s another important reason why vaginal microbiome screening should be a practice for those that are interested in taking part in the screen, would benefit from it and can afford it.”
Daye’s commitment to tackling the research gap in gynae health is certainly laudable but at £70-90 per test it feels like a tough sell. If you’ve got a bit of extra cash on your hands and you’re interested in understanding a bit more about what’s going on down there, getting your vaginal microbiome screened certainly isn’t going to do you any physical harm. But it’s also important to consider this product in the broader context of the gender health gap.
As Dr Morris adds: “The vagina has a delicate and healthy balance of bacteria which help to keep it free from infections such as thrush and bacterial vaginosis, and sometimes simple lifestyle changes can help maintain this balance, rather than paying for a test and treatment. There is a growing commercial market of feminine hygiene products that can actually disrupt microbiome. It is not necessary to use soaps or washing gels that can disrupt the microbiome. The vagina is self-cleaning and should be gently cleaned with either water, oils or emollients.
“We would encourage women to always consult their healthcare professional with any concerns that they have about their vulva and vaginal health, and they will be able to advise whether any treatment is required.”
Like what you see? How about some more R29 goodness, right here?