
Welcome to Sun Blocked, Refinery29’s global call to action to wake up to the serious dangers of tanning. No lectures or shaming, we promise. Instead, our goal is to arm you with the facts you need to protect your skin to the best of your ability, because there’s no such thing as safe sun.
One thing I’ve known about my body since I was little is that I have a lot of moles. So has my mother, as did her father, and with every year I’ve noticed more joining the gang. I’ve got moles on my face, red ones, brown ones, light ones, and even a cluster on my arm reminiscent of the Plough constellation.
To be truthful, I’ve never given them much thought. But working in the beauty industry and seeing the increasing awareness and conversations around sun damage and skin has meant that more recently, my moles have taken up residence as a niggling thought at the back of my mind.
I first heard of mole mapping a few years back (in a Peep Show episode no less). It’s a computer-assisted approach that enlists imaging technology to count and take pictures of moles, ruling out skin cancer. I added it to my growing list of ‘things I should do for my health’ before filing it away to be addressed at an unconfirmed later date. After all, I reasoned, my grandad had lived to be 98, worked on farms for his whole life and likely never knew what factor 50 was. Plus, my exposure to the sun is fleeting and sporadic so my risk had to be minimal. Right? It turns out that I shouldn’t have been so sure. But more on that later.
What are moles — and what causes them?
While many people have moles, not all of us (myself included) are sure what they are or why they show up. “Moles are common on the skin and form when pigment-producing cells group together,” says consultant dermatologist and British Skin Foundation spokesperson Dr Zainab Laftah. “They usually present in childhood or teen years but some appear later,” she says. There are different kinds of moles, too. “They can be flat and dark, slightly raised and coloured, or flesh-coloured and raised,” she explains.
How our moles develop and the number we accrue through life can be attributed to two things: genetics and our exposure to the sun. You can’t avoid your inherited disposition to moles but sun exposure can increase the number that appear, especially with more time spent in the sun during childhood, Dr Laftah tells me.
UV radiation is the most common cause of melanoma, a type of skin cancer which can spread to other parts of the body. According to research carried out by Macmillan and Soltan, 65% of us are unaware that exposure to UVA — one type of ultraviolet light emitted by the sun — can increase the risk of moles becoming cancerous. Crucially, we need wider education and increased awareness about moles: How to check them, which concerns to look out for, and how dangerous sun exposure can be.
When are moles a cause for concern?
Although the majority of moles are ‘normal’ or benign, they can change over time and turn into melanomas aka skin cancer. Contrary to popular belief, people around my age (26) aren’t exempt, as I learned from Professor Firas Al-Niaimi, a leading dermatologist and skin expert at Taktouk Clinic. In fact, Cancer Research UK reports that melanomas and carcinomas are the most common diagnosed cancers among young people. Dr Al-Niaimi added that just a few episodes of severe sunburn can increase your risk of developing melanoma. Similarly, just one session on a sunbed before the age of 35 increases your risk of developing melanoma by 75%.
This is not a lecture, and none of this is meant to scare you. But if I’ve learned anything from the many skincare experts I’ve spoken to over the years, it’s that keeping track of your moles is vital. “We usually say that if a mole is increasing, becoming asymmetrical or changing colour, please get that checked,” Dr Al-Niaimi tells me. So if, like me, you’ve got more moles than you can poke a stick at, then getting mole-mapped might be a seriously worthwhile investment for your health and peace of mind.
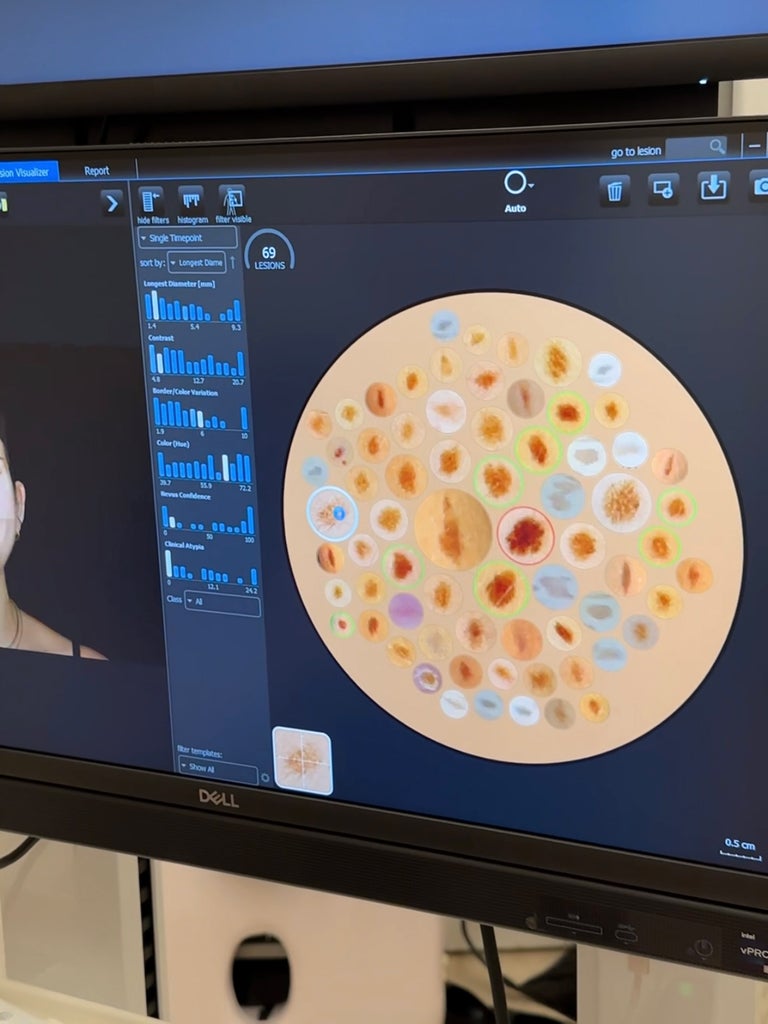
My mole count came to 69 in total. There they were, clustered together on the screen like a petri dish. Seeing them up close — the sheer volume of them laid out in that way — was unnerving.
What is mole mapping?
Mole mapping is a kind of skin health MOT that involves taking full body photographs using a camera to collate data on your moles, helping you and your dermatologist keep track of them and any changes to their appearance.
Depending on where you go, mole mapping services will utilise different technologies and software. To test out one of the most advanced mole mapping machines available in the UK, I headed to London’s Montrose Clinic to put my moles under the scrutiny of its Canfield AI machine.
What happens when you get your moles mapped?
For the admin-adverse (and those on a tight schedule), it’s good to know that the preparation for a mole mapping appointment is minimal. There’s no full-body shave or fake tan removal necessary, just a quick medical history form to fill out prior. The whole appointment took under half an hour, with the mole mapping itself taking around 15 minutes. This makes it easy to slot an appointment into your lunch hour and still have time to grab a sandwich afterwards.

When I arrived I was greeted by Ciara Vereker, a specialist nurse practitioner at Montrose and NHS lead skin cancer clinical nurse specialist for Imperial College Trust, who would be taking me through my mole mapping appointment. She explained what to expect, including how the camera works and what it would be able to show me. As it’s a comprehensive full-body scan, you can only wear your underwear for the photos in order to get the clearest possible results (one to note if you’re like me and often forget to wear a bra).
I stood on a marked spot in front of the head-height Canfield machine while Vereker talked me through the various poses I needed to take for the camera to get all the angles it required: facing forward, backwards, running man, inner leg, soles of my feet, hands behind head — nothing strenuous or reminiscent of a yoga class, thankfully. The camera whizzed through the different shots, taking detailed photographs of each section of my body. The AI present in this machine is instantly able to count and assess different aspects of the moles such as their colour, diameter, border and colour variation, as well as ‘clinical atypia’ aka how different from ‘normal’ a mole is.
My mole count came to 69 in total, which Vereker showed me on the Canfield’s computer. There they were, clustered together on the screen like a petri dish. I’ve been pretty comfortable with my moles my whole life but seeing them up close — and the sheer volume of them laid out in that way — was unnerving. That said, it granted me unparalleled 360-degree mole vision, allowing me to see ones I’d never laid eyes on before, including a mole at the back of my neck that had slightly concerned me as I’m forever catching it on my necklaces.
I couldn’t help but think back to the previous summer when I’d sunburnt my arms and noticed the skin around that mole peeling.
My moles also classed me as a strong contender for atypical mole syndrome, a disorder of the skin characterised by the presence of more than 50 moles, with three or more of them looking atypical. Vereker started selecting several moles for us to look at more closely on the screen. Of those 69 moles, she went over certain ones again based on what the machine had flagged as being of interest, as well as any that I wanted to check. For this second check, she used a hand-held camera that captured the moles in almost microscopic detail, showing them to me on the screen as she went along and assigning them each a status. ‘Inoffensive’ or ‘no remark’ meant I was good for another year; ‘follow up’ meant I would need to get them checked again in around four to six months.
Vereker explained that an annual mole check-up is recommended for most people, especially those at higher risk of melanoma, such as people with fair skin, skin that burns easily, those with a long-term history of sun exposure, sunbed users and people with a family history of skin cancer. A dermatologist may then flag concerning moles for ‘follow-ups’. While I hadn’t been seriously worried about any of my moles, the one I had singled out to Vereker as a possible concern (I’d noticed it was marginally darker and larger than my others) was one that the machine flagged. Visible differences in moles can be small and difficult to spot with the naked eye.
On closer inspection with the hand-held camera, Vereker assessed my moles using what’s known as the ABCD rule. Dr Al-Niaimi outlines the changes that specialists look for according to this guideline: “A is for asymmetry, so if there is asymmetry the two halves are not similar to each other and one half is changing. B is for borders, so if your mole starts to get an irregular-looking border. C stands for colour change — if it starts to darken, become black, grey or blue. D is for diameter, so if it’s increasing [in size].”
My rogue mole, located on my inner bicep, was looking slightly abnormal in its border and colour. It had grown to the size of a pencil-head eraser (I’d noticed it was only about half the size before), with a speckled, asymmetrical border and a darker, slightly raised centre. While these abnormalities weren’t obvious to my naked eye, they were glaringly apparent when I saw them under the lens of the machine. It drove home how vital mole mapping services and expert opinions are, even for those who think they can monitor their moles on their own.
Vereker explained that she would send the results straight through to the in-clinic dermatologist to have a look over, who would then discuss it with me in more depth. Five minutes later I was in dermatologist Dr Mariana Noy’s office. She explained what was concerning about my mole and recommended that, having further evaluated the mole herself, it would be best to get it completely removed. Dr Noy told me that the clinic could carry out the procedure with its in-house plastic surgeon as soon as the following day.
Being at risk of having a malignant mole at 26 was not on my bingo card for this year. But if it can happen to me, it can happen to anyone.
I’ll be honest, I was a little shocked. I’d come along to the appointment expecting to learn a bit more about my skin and to educate myself on moles; now I was being told that one of my moles was concerning enough to warrant full removal. I was so grateful that I was in such good care and that my concerns could be actioned straightaway by a dedicated team, but it did feel like a bolt out of the blue. I couldn’t help but feel uneasy afterwards: If I hadn’t been fortunate enough to have had this mole mapping service, I doubt I would have been concerned enough about that mole to get it checked out on my own.
While I’ve never used sunbeds, possibly get a holiday in the sun once a year if I’m lucky, and try to use SPF diligently, I couldn’t help but think back to the previous summer when I’d sunburnt my arms and noticed the skin around that mole peeling. It made me wonder if that was the trigger, and just how easy it is for one accidental sunburn to have a serious effect.

Being at risk of having a malignant mole at 26 was not on my bingo card for this year. But if it can happen to me, it can happen to anyone. Having only ever been seen by the NHS for medical issues, it was a completely new experience for me to be able to see my results straightaway and for them to be evaluated so swiftly by a medical professional with immediately actionable points.
How much does mole mapping cost?
The price for private mole mapping will depend on the type of service available in your area. Montrose Clinic’s package, which includes the mole mapping service with the Canfield IntelliStudio followed by a review with a consultant dermatologist, is £495. It goes without saying that access to private consultations and services such as these is a huge privilege, and it’s paramount to note that they aren’t easily accessible to individuals from all socioeconomic backgrounds. According to Cancer Research UK, around “4,000 cases of melanoma skin cancer each year in England are linked with lower deprivation” and with GP appointments notoriously difficult to secure, it puts those who aren’t able to afford private care at a huge disadvantage.
While melanoma incidence rates in the UK have increased by almost a third (31%) over the last decade, the good news is that education and intervention around skin cancer and the risks of sun exposure are being taken much more seriously. More NHS mole mapping services are being rolled out across the country, with medical practitioners including Vereker advocating for accessible mole screening to become a fundamental part of what the NHS offers. Beauty brands such as Hello Sunday are also doing their part, joining the drive to end VAT on sunscreen products and offering year-round VAT-free products to promote more accessible suncare for all. Boots is also running a mole scanning service, operated by initiative ScreenCancer, which is available in selected stores and starts at £40 for an individual mole scan.
For full transparency, I’ll be going to my NHS GP for an urgent referral for my own mole removal — though I’m still waiting for an appointment. While I was incredibly happy with the service at Montrose, my current financial situation won’t stretch to private removal, which starts at around £495, with an extra £250 to have the mole sent off for lab testing. The lesson this experience taught me — that even if you are only slightly concerned about a mole, and don’t think it’s a big deal, you should get it looked at — is priceless. If sharing my experience leads to more people getting their moles checked out, then it’s completely worth it.
When it comes to looking after your moles on a day-to-day basis, Dr Laftah suggests applying a broad spectrum sunscreen of at least SPF 30 daily. “Also avoid excessive sun exposure and remember to perform self-checks on moles for any changes,” she says. For moles that aren’t easily visible (i.e. those on your back), asking a friend or partner to take a photo of those areas every few months is important to be able to monitor any changes.
Another positive outcome of my appointment is that a handful of my friends are looking into getting their moles checked. It’s crucial to have these open conversations around skin cancer and if you are concerned, don’t put off getting a mole checked by your GP — or dermatologist if you can afford it. And please, the next time you’re out in the sun with your friends, make sure you’re all regularly slathering on the SPF.
Like what you see? How about some more R29 goodness, right here?
Why Do Brands Sell Tan Activators Knowing Risks?