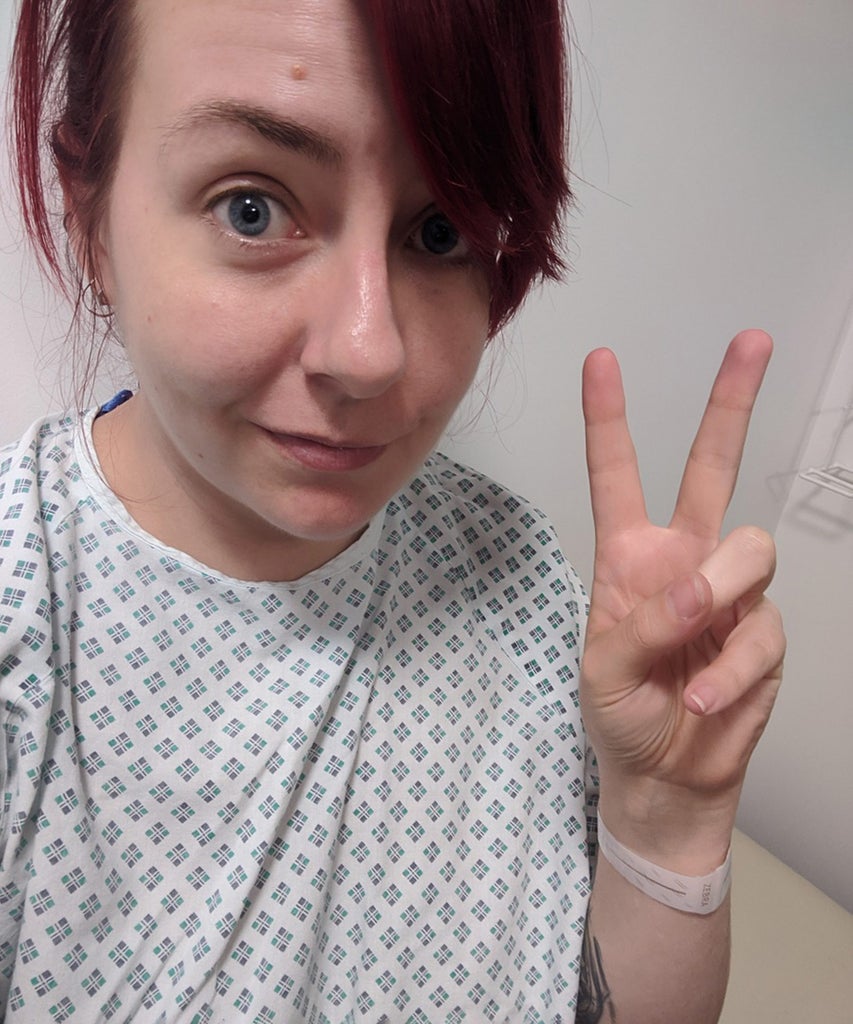
I never imagined I could be excited about having an operation. Hanging about a cold hospital in paper knickers before waking up to a sore stomach full of stitches is not really my idea of a good time but I’d been waiting for this day for years. Like every woman who has surgery for endometriosis, I hoped the experience would be worth it if it meant I could live some semblance of a pain-free life afterwards.
As is the case for most endometriosis surgery first-timers, I was having a diagnostic laparoscopy with a ‘see and treat’ approach. This meant that the medical team would have a look inside me and if they found any endometrium (the errant womb lining that attaches itself to the pelvic area instead of vacating during a period, which endometriosis sufferers are plagued by), they’d get rid of it.
Of course, though, there’s a bit more to it than that. Dr Leila Frodsham, consultant gynaecologist and spokesperson for the Royal College of Obstetricians and Gynaecologists, explains the procedure in more detail. “First of all, you’ll be given a general anaesthetic, so you’ll be asleep during the operation. The surgeon will then drain your bladder with a catheter before inserting a fine needle through your belly button. They pump carbon dioxide through this to fill your abdomen, separating your tummy wall from the bowel – this makes it easier for the team to look around. One or two other small incisions will be made – usually on the bikini line and just inside the belly button – and a tiny camera will be inserted, which is used to take photos or video of the condition, as well as act as eyes for the surgeon if any removal needs to take place.”
Like every woman who has surgery for endometriosis, I hoped the experience would be worth it if it meant I could live some semblance of a pain-free life afterwards.
Exactly how the endometrium is removed depends on a number of factors, such as where it’s located, its severity and the hospital’s own policies. Simply cutting out the tissue can cause bleeding, explains Dr Frodsham, so heat and lasers are often used at the same time to minimise damage. Once this is done, the incisions will be sewn up, painkillers administered and the anaesthesia withdrawn.
I’ll be honest, coming around from general anaesthetic is a slightly baffling experience – I immediately burst into tears, for example, even though I felt like I’d had the best nap ever – but there will be plenty of nurses on hand to get you reacquainted with reality.
Side note: take good snacks! You won’t be able to eat or drink for at least eight hours before your surgery but afterwards you’re likely to be ravenous, and a sad hospital sandwich is definitely not the self-care you’ll need at that point.
Most diagnostic laparoscopies for endometriosis are done as a day procedure, so you’ll arrive early in the morning to get prepped (7am in my case) and will be discharged that afternoon or evening, as long as there are no serious complications. Fortunately, these are rare. “All surgery involving general anaesthetic involves risk but laparoscopic surgery is minimally invasive,” says Dr Frodsham.
“It is possible for women to experience perforation of the uterus, bleeding inside the tummy, blood clots in the leg or lung, and bladder or bowel perforation, but these are uncommon. For diagnostic procedures – with no burning or cutting inside – the risk of damage to organs is one in a thousand,” she adds.
Don’t worry, as you’re getting ready for surgery (and doing things like giving urine samples and being fitted for fetching thrombosis socks), your surgeon will visit you to run through the risks and potential complications – don’t be afraid to ask questions if you’re unsure of anything.
There are no guarantees that the endometrium won’t grow back, nor that the surgery will alleviate all of my symptoms, but in the days after the operation I could certainly sense a difference in the way I felt overall.
Once you’ve been given the all clear, you’ll be allowed to go home (you’ll need to have someone pick you up and stay with you overnight). You’ll also be given instructions for caring for your wound sites, depending on the type of stitches you have. Because my endometriosis had spread itself across my pelvic region, I ended up having four small incisions, each about a centimetre in diameter, and each with removable sutures that I wasn’t allowed to get wet. This meant I couldn’t have a proper shower until they were removed at my GP’s surgery five days later, so you might want to stock up on wet wipes and dry shampoo. More fortunate souls might be given dissolvable stitches – your surgeon will explain what you need to do.

Most women will need a week off work after the surgery, although it could be as much as three to six weeks if you’ve had extensive removal (again, your surgeon will debrief you after the op). In any case, do not underestimate how knackered you’re going to feel. Shuffling around the house after this procedure is exhausting and while you could probably manage on your own, having a team of friends and family around to make tea, fetch stuff and just generally coo over you is invaluable for the first couple of days (although make sure they give you space – it’s not uncommon to feel unusually emotional after the procedure, and you’ll be napping a lot).
Physically, you’re going to feel sore around the wound sites and moving will be a bit of a challenge. You’ll be given some pretty generic painkillers; keep on top of them and take them regularly – you don’t want to play catch-up with the pain (which will ease off after a day or two). You might also have a sore throat from the anaesthetic tube – throat lozenges will help – and some vaginal bleeding – use a pad, not a tampon. Also, because you’ve essentially been pumped full of gas like a balloon, you’re going to be pretty burpy. Shoulder pain is not uncommon, either, since the gas can irritate nerves in the area. Gentle movement and stretching can help to relieve these symptoms.
Keep a close eye on your wound sites as women commonly report infection after a laparoscopy. Annoyingly, I was one of those women. If it looks like the wounds are not healing properly, are particularly red and inflamed, smell weird or feel hot, go to your GP. For me, a simple course of antibiotics sorted things out.
While endometriosis is linked to your time of the month, it’s not a period-specific condition. This meant that many of the symptoms were liable to flare up at any given point during my cycle. While my periods were generally horrendous and would regularly leave me writhing on the floor in agony, I experienced deep-rooted aches almost 24/7 in my legs and shooting pains in the lower back and pelvic area whenever I had sex or even just twisted awkwardly on the couch. And that telltale cramping you get just before your period? I had it constantly. You learn to live with the pain eventually but it’s exhausting – a tiredness that runs into your bones.
It’s been about six months since I had the surgery and while my symptoms are much improved, they are still there – although, thankfully, to a much lesser degree. I’m not spending hours on the toilet every time my period rolls around and I’ve not vomited from the pain once (which used to happen all the time). The aching in my legs is more of a background annoyance than a deafening assault on daily existence, sex is more comfortable, and the initial onslaught of pain during my period dissipates faster. Nor am I popping as many painkillers as before. But because so little is really understood about the condition, there’s no way of telling whether this is my new normal or whether things will gradually deteriorate and I’ll need surgery again in the future. Many women do.
Besides the infection, my surgery was by all accounts fairly textbook, although you’re no doubt aware that there’s a shocking lack of information about what ‘textbook’ actually constitutes because far too little is known about endometriosis. There are no guarantees that the endometrium won’t grow back, nor that the surgery will alleviate all of my symptoms long-term but, for now, I’m enjoying not being a slave to my own treacherous body.
Like what you see? How about some more R29 goodness, right here?
My Urgent Endometriosis Surgery Was Cancelled